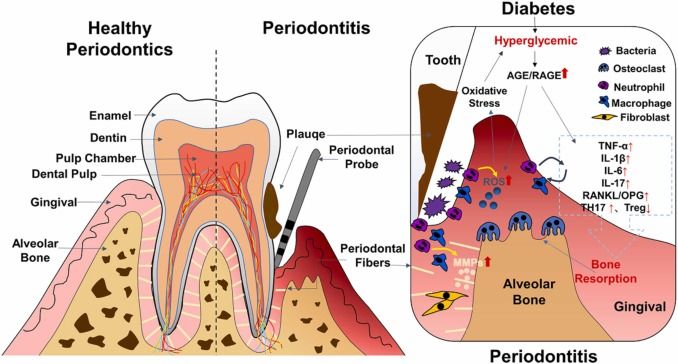
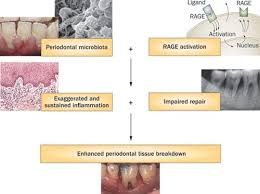
"Periodontitis and diabetes have a bidirectional link, making therapeutic treatment of periodontitis and diabetes challenging. Numerous factors, including microbes, inflammatory cytokines, immune cell activity, glucose levels, and metabolic disorders, contribute to the bidirectional relationship of periodontitis and diabetes. Basic periodontal treatment, medication, surgical treatment, and combined treatment are the most widely used treatments, but their efficacy are limited."Source
The individual host immune response to periodontal pathogens is very important. Systemic diseases and conditions alter host tissues and physiology which may impair the host's barrier function and immune defense against periodontal pathogens.
In simple terms, systemic diseases conditions themselves do not cause periodontitis.
Endocrine Disorders and Hormonal Changes;
1- Diabetes mellitus
2- Female Sex Hormones
3- Hyperparathyroidism
Diabetes Mellitus
It is a form of complex metabolic disorders which has to do with chronic hyperglycaemia as a result of diminished insulin production, impaired insulin action or even a combination of both
Two major types of diabetes
1- Type 1 diabetes mellitus
It is regarded as insulin dependent diabetes mellitus (IDDM) which is caused by a cell-mediated autoimmune destruction of the insulin-producing cells of the islets of Langerhans in the pancreas and as such brings about insulin deficiency and deficit.
This type has a marked tendency towards ketosis and coma. To compensate for the lack of insulin secretion by the pancreas, insulin injection could be prescribed by a medical professional.
Type 1 is also known as children's type of diabetes since it affects them in most cases
2- Type 2 diabetes mellitus
It is regarded as non insulin dependent diabetes mellitus (NIDDM) which is caused by peripheral resistance to insulin action and results in lack of storage of glucose in the tissues. This makes the quantity of glucose in the blood to be more than normal and eventually leads to hyperglycaemia.
In this case, the beta cells are not neutralised or taken out by cell mediated autoimmune deficiency. It typically begins as insulin resistance and later results to reduce production of insulin as the demand increases.
However, this is very common in obese individuals and can be often controlled and corrected by longer fasting periods and administration of oral hypoglycemic agents.
Oral Manifestations
i- Cheilosis
ii- Drying mucosa and cracking with fissures (dry mouth)
iii- Burning mouth and tongue
iv- Diminished salivary flow
v- Increased rate of dental caries in poorly controlled diabetic patient
vi- Changes in the normal flora of the mouth with greater predominance of Candida albicans, hemolytic streptococci and staphylococci and other opportunistic microbes
However, these symptoms are not always present and are not specific for a diabetic patient and therefore they are not pathognomonic for diabetes.
Periodontal manifestation include; tendency towards enlarged gingival tissues, sessile or pedunculated polyps of the gingiva, gingival proliferations, abscess formation, loosened teeth, delayed healing, periodontitis among others.
Periodontal disease is widely considered to be the sixth among complications of diabetes
Periodontitis in patients of type 1 usually appears at the age of 12 years.
Diabetes mellitus does not cause gingivitis or periodontitis but it alters the the response of the response of the periodontal response to local information of microbial plaque.
The altered response leads to the following in mode cases; increase rate of bone loss, greater attachment loss, increased bleeding on probing, increased tooth mobility, delayed post surgical healing and frequent periodontal abscesses occurrence.
These characteristics could be minimised or curbed completely in a controlled diabetic patient before the removal of local factors can yield positive response.
That's all as regards diabetic impact on periodontal tissues. More incoming reviews in the other incoming posts and happy reading.
Happy Blogging and Reading 💥💥💥💥
Video from umichdent YouTuber